Medical Billing and Coding Professionals Healthcare and IT Company
Provider Credentialing Services In Florida USA
In healthcare, provider credentialing is the process of verifying a provider’s professional background, including board certifications, hospital privileges, education, work history, insurance, and references.
This crucial step ensures patient safety, minimizes risks, and maintains compliance with industry standards.
Efficient Provider Credentialing Services in Florida for Your Practice
MDBC Pro provides fast and reliable provider credentialing services in Florida, helping physicians stay focused on delivering quality patient care.
Our skilled Credentialing Specialists carefully collect all necessary information from providers, often through a designated contact at your practice.
Additionally, our team ensures every detail is accurately prepared and submitted, making the medical credentialing services in Florida process smooth, timely, and hassle-free.
Why Florida Providers Need Credentialing Services
Proper provider credentialing services in Florida are essential for every healthcare practice. Here’s why they matter:
Ensure Compliance with Insurance Requirements: Credentialing ensures your providers meet all requirements for Medicare, Medicaid, and commercial insurers, helping prevent rejected claims and keeping your practice fully compliant.
Minimize Risk and Avoid Denials: Errors in credentialing can lead to claim denials, delayed payments, and compliance issues. Professional services make sure applications are accurate, verified, and meet payer standards.
Expand Your Payer Network: Credentialing allows your practice to join multiple insurance networks, increasing patient access and revenue. Navigating these requirements can be complex, but insurance credentialing services Florida like MDBC Pro simplify the process and ensure faster approvals with major insurers.
Save Staff Time and Resources: Credentialing is time-consuming. Outsourcing to experts reduces administrative work, allowing your staff to focus on patient care while ensuring applications are submitted accurately and on time.
- Stay Up-to-Date with Changing Rules: Insurance requirements frequently change. Expert credentialing services help your practice stay current, avoid compliance issues, and maintain continuous network participation.
Key Physician Credentialing in Florida for Major Insurance Payers and How MDBC Pro Handles Them
MDBC Pro provides expert Healthcare provider enrollment Florida, handling credentialing requirements for major payers and networks efficiently. Here’s how we support your practice:
UnitedHealthcare (UHC):
UHC requires providers to submit documentation via Onboarding Pro, including NPI, W‑9, licensing, education, liability insurance, and CAQH access. Primary source verification is also required. MDBC Pro prepares and submits all necessary documents, performs primary source checks, and continuously tracks the application status to ensure timely completion and approval.
Medicaid Managed Care Plans (e.g., UHC Community Plan):
Florida Medicaid managed care plans require a current license, DEA (if applicable), malpractice insurance, background checks, employment history, and ownership disclosure. MDBC Pro manages the full Medicaid credentialing process, gathering documents, completing applications, verifying credentials, and monitoring progress until approval.
Aetna (Florida):
Aetna may require a Letter of Intent (LOI) for certain providers or groups, along with board certification verification, licensure, and NPDB checks. MDBC Pro prepares LOIs, completes Aetna’s credentialing applications, verifies board certifications, education, and licenses, and ensures all requirements are met before submission.
Sunshine Health (Florida Medicaid / MCO):
Sunshine Health requires licensing disclosure, NPDB/NPIS checks, background screening, and the ability to correct any credentialing errors. Our team collects all documentation, submits corrections when needed, monitors the process, and ensures re‑credentialing is completed accurately.
General Medicare (CMS):
Medicare credentialing involves completing CMS-855 forms via PECOS, submitting CAQH data, performing primary source verification, and maintaining compliance with federal rules. MDBC Pro handles CMS-855 submissions, PECOS enrollment, CAQH updates, and primary source verification to ensure full Medicare compliance.

Provider Credentialing Services Offered by MDBC Pro in Florida
MDBC Pro provides fast and reliable provider credentialing services in Florida, helping physicians stay focused on delivering quality patient care.
Our skilled Credentialing Specialists carefully collect all necessary information from providers, often through a designated contact at your practice.
Additionally, our team ensures every detail is accurately prepared and submitted, making the medical credentialing services in Florida process smooth, timely, and hassle-free. Our services are designed to save time, reduce errors, and support healthcare providers at every step.
Initial Enrollment / New Payer Credentialing:
Fast and accurate enrollment into new insurance networks to expand your practice reach.
Medicare Credentialing:
Complete handling of Medicare applications and PECOS submissions for full compliance.
Medicaid Managed Care Plan Credentialing:
Efficient enrollment with Florida Medicaid managed care plans, ensuring smooth approvals.
Commercial Payer Credentialing:
Credentialing with major insurers such as Aetna, UHC, and BCBS to maximize your network.
CAQH Profile Management & Attestation:
Accurate setup and timely attestation of CAQH profiles to prevent delays.
Primary Source Verification:
Verification of licenses, education, work history, and certifications to meet payer requirements.
Application Preparation and Submission:
Complete and accurate paperwork submission to reduce errors and speed approvals.
Re-Credentialing / Re-Validation:
Timely management of re-credentialing to keep providers active across networks.
Appeals and Follow-Up on Denials:
Resolving credentialing denials and rejections efficiently so providers can continue patient care.
Credentialing Data Tracking and Maintenance:
Organized tracking and management of provider information for seamless updates.
Sanctions Monitoring and OIG / Exclusion Screenings:
Ensuring compliance and avoiding potential payer issues with regular monitoring.
Provider Network Expansion Support:
Assistance in joining new insurance networks to grow your practice.
Payer Contract Onboarding Support:
Smooth onboarding and contracting with payers to prevent delays in approvals.

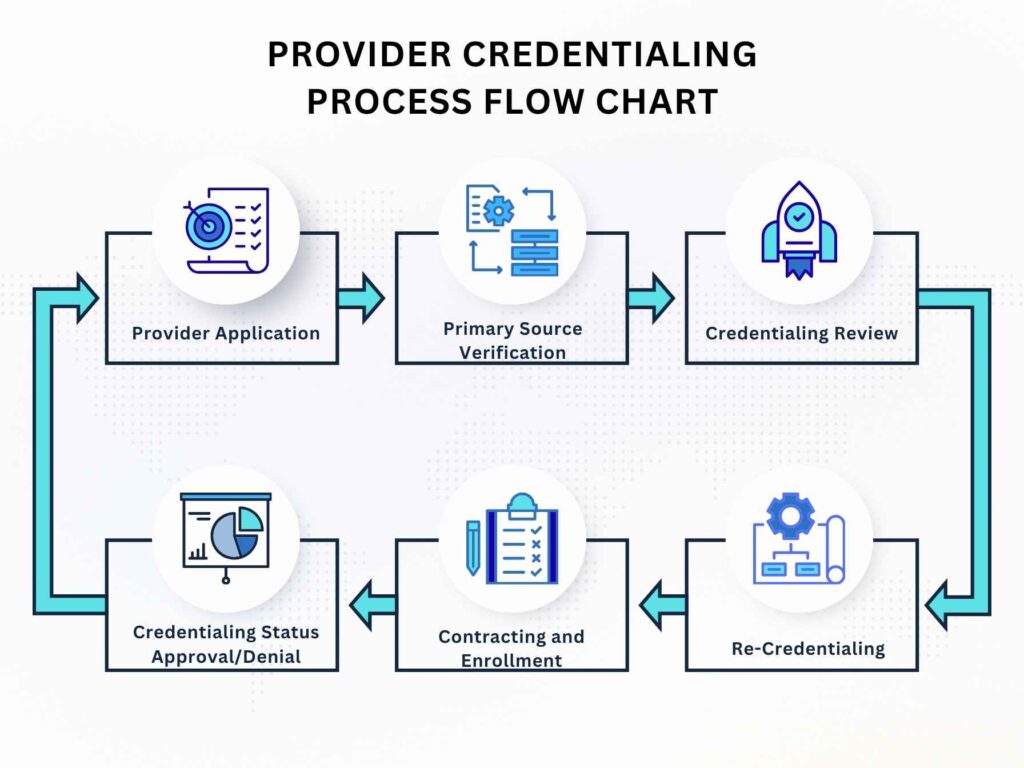
How do Our Medical credentialing services in Florida work?
- End-to-End Credentialing: MDBC Pro (Medical Billing and Coding Professionals) offers full support for Medicare and commercial payer enrollment through our reliable Physician credentialing in Florida, ensuring correct documentation and a smooth approval process.
Document Management: Working closely with clients to collect and organize all necessary documents, ensuring accuracy and timely submission throughout the credentialing process.
Database Setup: Keeping an organized provider database that tracks the status of all required documents.
Enrollment Form Processing: Accurately preparing and submitting insurance enrollment forms to ensure smooth approval by all carriers.
Follow-Up: Regularly tracking and communicating with insurance carriers until applications are fully approved.
Re-Credentialing Management: Monitoring providers to ensure timely re-credentialing and compliance.
Why Healthcare Providers Trust Credentialing Companies in Florida
MDBC Pro is one of the leading credentialing companies in Florida, providing expert provider credentialing services in Florida for physicians, hospitals, and healthcare organizations. Here’s why providers choose us:
Over 10+ Years of Credentialing Experience: With more than a decade of experience in Florida medical provider credentialing, our team understands the nuances of the credentialing process for providers in Florida and ensures applications are handled efficiently and accurately.
Skilled Credentialing Specialists: Our certified specialists manage every step of physician credentialing Florida, from initial enrollment to re-credentialing, ensuring compliance with all payer requirements and reducing errors.
Fast, Accurate, and Compliant Credentialing: We provide reliable healthcare provider enrollment Florida, ensuring all documents, applications, and verifications are submitted on time and meet payer and regulatory standards.
Hands-on Follow-Up and Appeals Management: Our team actively monitors applications, resolves any denials, and manages appeals, keeping your credentialing process smooth and minimizing delays.
Focus on Hassle-Free Credentialing: By handling all aspects of credentialing, including hospital credentialing Florida, we reduce administrative burdens so providers can focus on delivering quality patient care.

